What if you get diagnosed with cancer? What if your beloved family member, partner, or friend gets diagnosed with cancer? The news may fill you with fear and despair. Particularly, what if you get diagnosed with glioblastoma (GBM)? GBM is the most aggressive type of brain cancer with an average overall survival of 15~21 months after the first diagnosis. Moreover, GBM patients’ 5-year survival rate is less than 7%, one of the lowest among all cancers. Although treatment for other types of cancer is becoming more and more successful, current treatment options for GBM are largely ineffective and inevitably result in relapse and death. However, at the Laboratory of Cancer Epigenetics and Plasticity at Brown University and Rhode Island Hospital, we are working on innovative new treatments for GBM. One of these projects is called GliaTrap.
What’s Drug discovery process?
How does a new treatment get discovered? The drug discovery process is divided into three steps:
1. Drug Discovery and Development.
2. Preclinical Research
3. Clinical Research.

During Step 1, researchers elucidate the mechanisms of disease progression, which leads to the discovery and development of a treatment that inhibits the disease process. Once a potential therapeutic candidate is selected, this candidate will go to Step 2 where researchers test the safety, side effects, how the drug affects the body, how the body responds to the drug, and so forth. Preclinical research requires a different laboratory setting than an Academic Research Lab and it should be monitored by a third party (e.g. the FDA in the US). Once this therapeutic candidate is determined to be safe enough, then this treatment will go to Step 3, Clinical Research, where its efficacy in human patients will be tested. This entire process takes about 10-15 years for a single treatment candidate to become available to patients.
Current therapies for GBM include surgical removal, chemotherapy, radiation therapy, or a combination of those. Each treatment modality has its own advantages and disadvantages. Surgery removes most of the bulk tumor but it cannot remove individual cells, which remain in the brain. Chemotherapy is normally administered to treat these remaining GBM cells, however it is challenging to specifically target the distributed GBM cells without killing the surrounding healthy normal cells. Radiation therapy has similar disadvantages as chemotherapy since targeting only cancer cells without damaging the surrounding healthy normal cells is impossible. As explained above, all the current approaches face huge clinical challenges, which makes GBM currently impossible to treat.

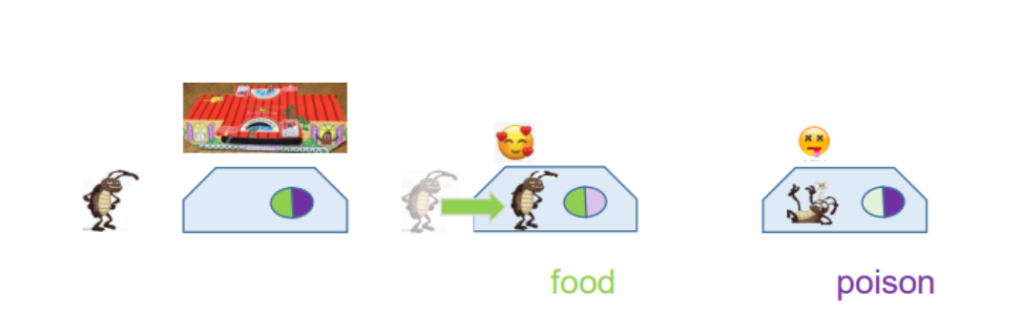
To address this challenge, we are developing a new technique for GBM therapy: GliaTrap. GliaTrap basically functions just like a Japanese cockroach trap “Gokiburi hoihoi”, a container that houses foods to attract cockroaches and drugs to kill the attracted cockroaches. For the concept of GliaTrap, you should think of cancer cells in the brain like the cockroaches in my example. (Figure 2). GliaTrap uses a biocompatible material called hydrogel, like the container of the Gokiburi hoihoi, to house food and drugs that lure and kill cancer cells. Food for cancer cells is called a chemoattractant, and GliaTrap uses this molecule to lure the residual GBM cells post-surgery to the vicinity of the empty space, just like a cockroach trap uses food to attract cockroaches. Once these cancer cells are attracted to GliaTrap, GliaTrap uses an anti-tumor agent to kill those cells at the vicinity of the empty space without causing significant damage to healthy cells, just like cockroach traps use drugs to kill the cockroaches. We hope that GliaTrap will be able to eliminate the remaining cancer cells from the surgery to prevent tumor recurrence.
GliaTrap can utilize not only anti-tumor agents, but also lure/use the body’s natural immune cells. Anti-tumor agents in GliaTrap can be replaced with immune cell activators, molecules that boost the ability of immune cells to attack cancer cells. GliaTrap can serve as a new treatment delivery method in concert with surgical removal and chemotherapy. GliaTrap combines targeted capture and drug release to increase therapeutic efficacy and safety by selectively killing the cancer cells that surgical removal and chemotherapy might miss. As a result, GliaTrap could increase the survival rate of GBM patients.
Looking forward, GliaTrap can potentially be applied to other types of invasive cancers that don’t have effective current treatments such as pancreatic cancer. Pancreatic cancer has a similar treatment protocol – surgical removal followed by chemotherapy, radiotherapy, or a combination of those. GliaTrap could be implanted into the empty space created by removal of pancreatic cancer cells, and perform in a similar way as described for GBM by choosing an optimal chemoattractant for pancreatic cancer cells. To ensure the coverage of capturing cancer cells, genetic profiles of cancer cells can be investigated and optimal chemoattractants can be utilized. Chemoattractants and therapies can be selected based on the genetic profiles of cancer patients, and GliaTrap can be tailor-made for each patient. With continued effort, GliaTrap could become a platform for combination therapies for various types of cancers contribute to personalized treatments options.

The GliaTrap project has great potential but as every paradigm shifting discovery, it comes with many challenges. It needs a lot more studies to prove its effectiveness and safety before it can be applied to patients. Ultimately, with our work at the Laboratory of Cancer Epigenetics and Plasticity, we hope to help patients and their loved ones to no longer view the diagnosis of cancer as a death sentence, but rather as a challenge that can be overcome with the right treatment.
References:
1. Louis, D. N. et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathologica 131, 803–820 (2016).
2. Toms, S. A., Kim, C. Y., Nicholas, G. & Ram, Z. Increased compliance with tumor treating fields therapy is prognostic for improved survival in the treatment of glioblastoma: a subgroup analysis of the EF-14 phase III trial. J Neurooncol 141, 467–473 (2019).
3. Wang T, Suita Y, Miriyala S, Dean J, Tapinos N, Shen J. Advances in Lipid-Based Nanoparticles for Cancer Chemoimmunotherapy. Pharmaceutics. 2021; 13(4):520. https://doi.org/10.3390/pharmaceutics13040520
4. Tapinos, N., Sarkar, A. & Martinez-Moreno, M. Systems and Methods for Attracting and Trapping Brain Cancer Cells. (2017).
One thought on “A new personalized cancer treatment – will ‘GliaTrap’ be able to lure and treat cancer cells to prevent tumor recurrence?”